Radial Keratotomy (RK) - Eyes needlessly damaged
"Indeed, those who fail to heed prior mistakes are doomed to repeat them—to the detriment of our patients and our professional reputations." (George Waring, MD, 1999)
RK was introduced into the United States in 1978 without proper scientific assessment of long-term safety and efficacy. The RK technique consisted of radial corneal incisions made manually with a blade. In the 1980's, widespread concern about the procedure began to build and RK was eventually abandoned to the junk heap of refractive surgeries. Will LASIK be next?
"It is well documented that RK incisions never completely heal..." (Nassaralla et al, 2007)
Like the LASIK flap, RK incisions never heal and remain open for the rest of a patient's life. This situation exposes RK patients to a life-long increased risk for corneal infection and even internal ocular inflammation and infection. RK patients who develop untreatable infections may be required to undergo corneal transplant, sometimes even many years after RK.
Patients who suffer from problems after RK are invited to join the discussion on FaceBook.
Images on this page were provided courtesy of Dr. Edward Boshnick, who has devoted his practice to the restoration of quality vision and comfort after RK, LASIK, and other forms of refractive eye surgery. Many of the photos below were taken after dye was instilled into the eye, which highlights diseased or injured tissue under a special light.
Eye doctor ordered to pay $5.6 M after "negligent" vision-correction surgery ends dentist's career - National Post 10/17/2019
From the article: Wearing thick-lensed glasses, Brent Jesperson had no problem performing his work as a dentist. Playing sports with the Coke-bottle spectacles on was another matter. So Jesperson jumped at the chance to undergo the first generation of vision-correction surgery in 1994, especially after his chosen ophthalmologist suggested the risks were minimal. The “radial keratotomy (RK)” seemed to be a success at first, but over the years his eyesight actually worsened, with blurriness in one eye, glare and impaired depth perception. Finally, unable to work on patients and feeling depressed and suicidal, Jesperson abandoned his lucrative dental practice in 2009.
Canadians suffering severe complications after radial keratotomy eye surgeries - CTV News 1/13/2019
From the article: Today, however, this once-celebrated treatment has largely been abandoned, in part because of questions over its safety...
Dr. Edward Boshnick is a Miami-based optometrist who specializes in treating those who have experienced vision loss or discomfort from past eye surgeries. It’s not uncommon, he says, for RK patients to develop complications long after undergoing the procedure.
“After the surgery is done, that cornea can change shape, so it doesn’t have the same rigidity,” he told CTV News. “A lot of these patients, maybe most of them, became very farsighted and very astigmatic because the irregularity of the cornea increased.”
Other RK complications, Boshnick explained, can include “dry eye, ocular pain… glare, halos, multiple vision.”
Added 9/3/2016. The following article was written by an optometrist and published in the Times Leader newspaper in 1994.
THERE IS NO ERASER AT THE END OF A SCALPEL. Radial keratotomy, the unkindest cut.
Thursday, February 10, 1994
By Dr. JOSEPH H. SMITH
A few years ago I started collecting anecdotes about radial keratotomy, an eye surgery that promises nearsighted people a life without glasses. Then I realized that radial keratotomy is no joke.
Something is wrong!
Radial keratotomy, in my opinion, is an unnecessary procedure that is being driven by newspaper, magazine and television advertising, and that too often leads to sad complications.
I am an optometrist, not an eye surgeon. That means I often see patients in my practice after they have had this surgery. Several have had less-than-desirable outcomes; a few have been virtual disasters. Continue reading
Added 9/14/2014: The photo below is the eye of a patient who underwent RK in 1988. Sometime later the patient's vision deteriorated, and in 1998 the patient had LASIK surgery. You can see that both the RK incisions and the LASIK flap have not healed after all of these years. This patient sees 20/200 or worse, which is not correctable with glasses. The patient must wear a therapeutic hard contact lens which vaults over the entire cornea and rests on the white part (sclera) of the eye.
The photo below-left shows a post-RK cornea with dry eye disease. Cutting of the corneal nerves during RK and other forms of corneal refractive surgery commonly leads to chronic dry eyes. Click to enlarge.
The photo below-right shows a cornea with eight radial RK incisions and two horizontal, or t-cuts. These incisions never fully heal. Click to enlarge.
Addressing the post-RK hyperopic shift. Michelle Dalton. EyeWorld, August 2012
From the article: Unfortunately, it wasn't until the mid-1990s that published studies alerted surgeons to the long-term issues with RK, said Parag A. Majmudar, M.D., associate professor of ophthalmology, Rush University Medical Center, Chicago, and in private practice, Chicago Cornea Consultants Ltd.
"RK never stops," he said. "The incisions continue to flatten the cornea and that's what causes the hyperopic shift, and it's progressive. These patients are miserable most of the time."
John A. Vukich, M.D., partner, Davis Duehr Dean Center for Refractive Surgery, Madison, Wis., started performing RK in the early 1990s but had abandoned it by 1995. "Many of the RK patients who were in their early 30s at the time of surgery are now in their 50s. Most of them became presbyopic earlier because of latent hyperopia post-RK. Almost every one of them is back in spectacles and few are happy with their current vision," he said. "Unfortunately, these were patients we thought we were helping at the time."...
"Hyperopia of RK is the gift that keeps on giving," Dr. [Eric] Donnenfeld joked.
The photo below is an eye that had 2 RK surgeries followed later by LASIK. The white arrow points to one of the old, unhealed RK incisions. The red arrow points to the edge of the LASIK flap, which is also not healed. Green dye instilled in the eye settles into the surgical-wounds. The dye is illuminated under special light. Click photo to enlarge.
The two images below the photo are topographies of the patient's corneas. Blue areas represent relatively flat areas of the cornea. Red represents relatively steep areas. As you can see, the patient's corneas are very irregularly shaped. Click images to enlarge.
The photo below is an eye with long RK incisions within the patient's line of sight. These scars cause blur and visual distortion. RK incisions never fully heal, and place the patient at risk for future problems.
/RK-long-incisions(320).jpg)
The photo below is the eye of a patient who had RK in 1988 and later developed ectasia. You can see the radial pattern of RK cuts as well as a vertical cut to the left of the pupil. Dye instilled in the eye settles into the open incisions, demonstrating the cornea's inability to heal. You can also see what appears to be a bubble on the cornea which is where the cornea is bulging (circled in white on the right-hand image). This is corneal ectasia. Ectasia occurs when the cornea is too weak to withstand the constant outward force of normal intraocular pressure. The patient's vision can only be corrected to approximately 20/400 with glasses. Click photos to enlarge.
The photo below-left is the eye of a patient who had RK over twenty years ago. Years later an unknown bacteria or other opportunistic organism entered the cornea through one of the open RK incisions (white arrows point to old open RK incisions), resulting in a corneal infection. The infection led to vision loss and need for a corneal transplant (the red arrow points to the edge of the transplanted cornea, which appears as a crescent shape). Green dye was instilled in the eye to highlight irregularities of the cornea. The patient's vision is very poor and cannot be fully corrected with glasses. Click photo to enlarge.
The photo below-right is a photo showing old non-healed RK incisions. Click photo to enlarge.
RK and cataract surgery
Mark Packer, M.D. Phacoemulsification after radial keratotomy. EyeWorld, January 2012
From the article: Unfortunately, we now find ourselves dealing with this unintended legacy as we take care of an increasing number of post-RK presbyopic hyperopes and cataract patients... If a clear corneal [cataract] incision is made through an RK incision, there is a high likelihood that the roof of the [cataract] incision will split open along the RK incision due to manipulation during the course of the procedure. The split roof of the clear corneal incision will prevent a good seal at the incision and allow excessive outflow of fluid and consequent chamber instability during [cataract surgery]. An unstable chamber can lead to multiple complications including iris damage, endothelial damage, capsule rupture, and vitreous loss. A split incision roof can also lead to difficulty in closing the corneal incision at the end of the case. Often multiple sutures are required to achieve a watertight closure. The added sutures can create astigmatism and patient discomfort. A poorly sealing corneal incision may also increase the risk of endophthalmitis." (From Wikipedia - Endophthalmitis is an inflammation of the internal coats of the eye. It is a dreaded complication of all intraocular surgeries, particularly cataract surgery, with possible loss of vision and the eye itself.)
Sidebar: These patients need to be warned about the likelihood of a lens power calculation error and the greater surgical difficulty that the corneal incisions impose. ~ Kevin Miller, M.D.
The photo below-left is the eye of a patient who had RK with t-shaped incisions, followed by LASIK surgery. The green dye which was instilled into the eye settles into wounds which are not completely healed. Click image to enlarge.
In the photo below-right, old RK incisions (which never heal) can be seen deep in the visual axis (pupil area). These scars cause light rays to scatter and impair the patient's vision. Click image to enlarge.
The three images below are photos of the eye of a patient who had RK, followed by LASIK, and later developed corneal neovascularization as a result of these unnecessary surgeries. In the top left photo, you can see that the green dye which was instilled into the eye has settled into the open RK incisions and LASIK flap. This is evidence that the cornea never heals. You can also see that blood vessels are growing into the cornea (neovascularization), which is a sight-threatening situation. Click on images to enlarge.
The photo on the left below is the cornea of a patient who was nearly blinded by three separate RK surgeries 20 years ago. Multiple visible RK incisions remain open, which demonstrates the cornea's inability to heal. The corneal surface is very irregular, resulting in distorted, extremely poor vision. Due to the cornea's weakened state, the patient also developed corneal ectasia. Click image to enlarge.
The photo on the right below shows the cornea of a patient who had RK surgery in 1995 followed by LASIK in 2004. Both of the patient's corneas are extremely dry, and the corneal surface is highly irregular. The diseased cornea is irritated and blood vessels are growing into the cornea. (A healthy cornea is clear, and has no blood vessels). Note the LASIK flap margin at the 9:00 o'clock position, which demonstrates that the flap has not healed after all these years. The patient is wearing a large therapeutic contact lens. Click image to enlarge.
Below are two photos of the same eye (under different lighting). The patient originally had RK twenty years ago, followed by a 2nd RK surgery, and two LASIK surgeries. The edge of the LASIK flap and the RK incisions are still visible after many years, which demonstrates the cornea's inability to heal. This cornea is biomechanically unstable, and the optics of the eye are ruined from these surgeries. Click images to enlarge.
Case Report: Post-RK bullous keratopathy
The following three images show the cornea of a patient who underwent complicated RK surgery. The RK incision penetrated the cornea and damaged the endothelium on the back surface of the cornea, which functions as a pump to keep the cornea clear. The cornea was subsequently stitched leaving a scar. The damage to the endothelium caused the cornea to swell, eventually leading to separation of the epithelium (corneal front surface) from the underlying corneal tissue. The bubble-like circular area in the upper-left photo and green circled-area in the upper-right photo and is the location of the epithelial separation from the cornea, which is shown in the cross-sectional scan image at the bottom.
/post-RK-bullous-keratopathy.jpg)
/post-RK-bullous-keratopathy2.jpg)
/post-RK-bullous-keratopathy-scan.jpg)
The two photos directly below show the cornea of a patient who had RK surgery followed by LASIK surgery. Note the blood vessels growing from the white of the eye into the cornea at the 5 o'clock position. A normal cornea is transparent and avascular. This is disease state, known as corneal neovascularization, which is a direct result of the trauma to the cornea by these unnecessary, destructive surgeries. This patient's vision will be impaired if the blood vessels reach the visual field. In addition to the abnormal blood vessel growth, you can see the old RK incisions and the hazy ring around the corneal periphery which represents the LASIK flap margin.
/postRKpostLASIKneovascularization(320).jpg)
/postRKpostLASIKneovascularization2(320).jpg)
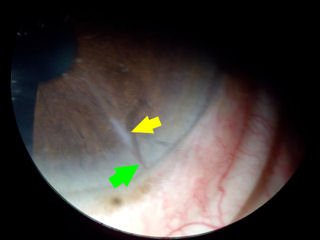
The image below-left is a close-up photo of an RK incision. The yellow arrow points to the dense incision scar. If you look closely at the tip of the green arrow, you can see blood vessel growth into the cornea at the location of the RK scar. Click on photo to enlarge.
The image below-right shows an eye with RK incisions. The green arrow points to blood vessel growth into the cornea at the 6:00 position. Click on photo to enlarge.
The photo below-left shows a post-RK cornea with open incisions and blood vessel growth into the cornea at 4:00 and 6:00. The patient is wearing a rigid scleral lens which is visible on the white of the eye. With the lens, the patient sees 20/20 without visual distortions.
.jpg)
The two images below are of eyes that have had both, RK and LASIK. The photos were taken through a slit lamp (bio-microscope) after applying fluorescein stain on the eye. The green-yellow circle around the periphery of the cornea is the LASIK flap edge. The spoke-pattern is the RK incisions, which are clearly visible. The LASIK flap edge and RK incisions are staining green-yellow because the dye settles into the wounds which are not completely healed.
.jpg)
.jpg)
The next four images below also demonstrate that RK incisions never heal. These open portals can allow opportunistic organisms to enter the eye causing infections and inflammation. The first two photos are corneas 20 years after RK. The patient in the 4th image (bottom right in this section) shows the cornea of a patient who had 2 RK procedures in 1989 followed by LASIK in 2000. The green color around the LASIK flap indicates an opening in the seam of the flap. The green dye in the RK incisions indicates that these incisions are still open and placing the patient at risk for infection and inflammation.
/rk-incisions-still-open-after-20yrs(s).jpg)
/20yr_postRK(320).jpg)
The image below-left is the eye of a patient who had a corneal transplant following botched RK. Note the RK incisions in the superior visual field. The transplant had to be placed off-center due to the long, deep incisions.
The photo below-right shows the eye of a patient who has very long, deep, wide RK scars. The patient is wearing a rigid scleral contact lens. The edge of the lens is visible on the white of the eye.
/post_RK_off_center_corneal_transplant(320).jpg)
/wideRKincisions(320).jpg)
Corneal ectasia can occur after Radial Keratotomy (RK) as well as after LASIK. The image below on the left shows the cornea of a patient with post-RK ectasia. The patient had RK in 1988. He began losing visual quality in 1990. In addition to the corneal protrusion, note the faint white spot at the apex of the curve. This is internal corneal tissue that is protruding out of one of the RK incisions.
The photograph below on the right is the cornea of a female patient who lost functional vision after RK 17 years ago. The RK incisions are unusually deep and long. Note how flat the cornea is along the visual axis with inferior steepening. The patient has recently been fit by Dr. Boshnick with a new specialty hard contact lens and has regained functional vision.
.jpg)
.jpg)
The next two photos show the cornea of a patient who had 2 RK surgeries followed by 2 LASIK surgeries. In the photo on the left, the patient is wearing a scleral lens.
/2RK2LASIKwithsclerallens(320).jpg)
/2RK2LASIK(320).jpg)
The photo below-left is the cornea of a 60 year old female patient who had 2 RK surgeries followed by 2 LASIK surgeries. With glasses, her visual acuity in this eye is 20/400. The photo was taken after instillation of a special dye that highlights diseased areas of the cornea. The green-yellow lines are open RK incisions. The ring around the periphery of the cornea is the edge of the LASIK flap, which will never fully heal. These open wounds place the patient at life-time risk of opportunistic bacteria and viruses penetrating the cornea, with potentially disastrous consequences.
The photo below-right is the cornea of a patient who has epithelial ingrowth following RK, RK enhancement, LASIK, and LASIK enhancement. The red arrow points to an RK incision that is still open. The green arrow points to the LASIK flap edge, which is not healed. The yellow arrow points to the pocket of epithelial ingrowth, which is a potentially sight-threatening complication. The patient has constant pain in addition to extremely blurred and distorted vision. Click on photo for a larger image.
The image below-left is a photograph of the cornea of a patient who had RK eighteen years ago. In addition to the open radial cuts, the patient has an open horizontal incision. The dark blue oval area surrounding the horizontal cut is an area of corneal steepening (ectasia). The patient's vision with and without glasses is very poor. The patient requires a large rigid contact lens which vaults over the irregular corneal surface.
The image below-right is an RK cornea with highly unusual cuts.
/18-years-post-RK-open-incision-and-ectasia-s.jpg)
/rk-unusual-cuts.jpg)
The photo below-left shows open RK incisions 18 years after surgery.
The image below-right shows another unusual RK cut pattern.
/rk-incisions-still-open-after-18yrs.jpg)
/rk-smiley-face.jpg)
The photo below shows a cornea with deep horizontal RK incisions in addition to radial incisions. Click image to enlarge.
The following images were acquired using a technique called optical coherence tomography, or OCT. The instrument produces a cross-sectional image by scanning the front of the eye (anterior segment) with a beam of light. Think of it like an ultrasound using light instead of sound waves to create an image of tissues.
The image below-left shows a cornea with very deep RK incisions. Note the incisions nearly penetrate the full thickness of the cornea. The image below-right shows a scleral lens on a post-RK cornea with open incisions. This cornea is unstable. Click on images for a larger view.
The two images directly below are photographs of the cornea of a female patient who had RK and consequently developed ectasia. This cornea is only 180 microns thick at the thinnest point. Average corneal thickness for normal eyes is approximately 550 microns. As you can see, the corneal surface is very irregular, which causes distorted vision. Click on the images for a larger view.
Below-left, the red arrow points to an old RK incision. Click image to enlarge.
Below-right is a post-RK, post-LASIK cornea wearing a hard contact lens. Click image to enlarge.
The image below on the left is a corneal topography of an eye that developed ectasia after RK and LASIK. This topography demonstrates a cornea with a very irregular surface full of hills and valleys and not smooth or spherical. The color blue represents the flatter areas of the cornea. Red represents the steepest area which is bulging or protruding. Corneal surface irregularity as illustrated results in visual distortion.
The image to the right is a corneal topography of a normal, unoperated eye for comparison.
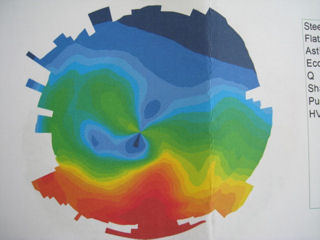

The two images below are corneal topographies of eyes that have undergone two separate RK procedures followed by two separate LASIK procedures. As you can see, these corneas are highly irregular.


Two "successful" RK procedures, followed by "successful" LASIK surgery, followed by LASIK enhancement
Delayed radial keratotomy dehiscence following uneventful cataract surgery
Excerpt: Previous RK not only complicates intraocular lens power selection due to unintentional postoperative hyperopia and postoperative hyperopic shift, but can also reduce corneal tensile strength. RK incision dehiscence has been reported during phacoemulsification cataract surgery, corneal transplantation and following blunt trauma including car airbag inflation. Previous reports suggest considerable variability in corneal strength following RK.

RK patient develops ectasia 10 years later, undergoes crosslinking which results in gaping of RK incisions
Editor's note: I read a case report of a post-RK patient who developed ectasia 10 years later. The patient was treated with corneal collagen crosslinking. On day 1 after crosslinking, the patient experienced intense pain. It was discovered that one of the RK incisions had opened up. On the fourth day after crosslinking, another incision opened up, and again on day 7 a third incision opened up. The patient was taken to the operating room where the open incisions were sutured closed. The patient subsequently developed haze and reopening of the incisions. Another surgery was required to resuture the incisions. Six months later the sutures were removed but the patient had severe scarring of the cornea, which remained one year later. See abstract below.
- - - - - - - - - - - - -
Gaping of radial and transverse corneal incisions occurring early after CXL.
J Cataract Refract Surg. 2011 Dec;37(12):2214-7.
Abad JC, Vargas A.
Abstract
A 33-year-old woman with corneal ectasia after radial and astigmatic keratotomy had corneal collagen crosslinking with resultant gaping of the inferior incisions (2 radials and 1 transverse) that required suturing. At 6 months, the incisions healed leaving fibrotic scars. Visual acuity, refractions, corneal photographs, and topographic and corneal wavefront measurements are presented. At 2.5 years, the topographic inferior corneal irregularity continued to improve.
RK patient complaint to FDA, vision deteriorating over many years
Excerpt: By 2010, I started noticing that my eyes were deteriorating rapidly and I went back to see Dr [redacted]. Dr [redacted] put me back in glasses -but they didn't work for me. Dr [redacted] currently has me using contact lenses which are helping a little bit, but they are not correcting my problem. I am slowly going blind and was told there is nothing that can be done to correct the damage that was done by Dr [redacted] in 1993. I am a [redacted] contractor, I have never been married nor do I have any children. I am self employed which is my only means of support. Once I have totally lost my eye sight, which I have been told is a very short time away, I have no means of income. Read full report
FDA complaint 15 years after RK
At [redacted], in 1995, I chose refractive eye surgery called RK. It was a [redacted] copay per eye at the time and although a bit radical, even scary, the testimonials and advertising of the day were convincing. The benefit was amazing, for 12 to 13 yrs, then things began going south. An attempt to return to glasses for correcting the mono-vision that I had were impossible to use. So they were put away and I just continued to cope with deteriorating vision. Nothing dramatic, just fuzzy. I had no idea that my RK decision had enrolled me in a club that I didn't want to be a part of. Folks that were led down the primrosed path of corrective eye surgery without studies that plainly indicated the future complications. Three weeks ago I woke to find I could not read the time 8 feet away. Fortunately that was a morning thing and hasn't repeated too often. However, I've learned that my eyes are now left 20/60 and right 20/150 for distance and the right eye, my reading eye, is 20/30 for reading. I'm [redacted] retired and just finished out my vision [redacted] insurance on the last of Oct. [paste in a frown]. The important part is that I'm discovering and reading much about the entire post RK population and problems online. I can see that I've paid my dues and Ii am a full fledged member with an unk future. Source
FDA complaint: Complications emerge 14 years after RK
Radial keratotomy complications 14 years after surgery. Halos, ghosting, shadows, blurring, starburst, diminished contrast, depth, and night vision, dizziness, photophobia, rapid degeneration of eyesight. Rapid decline of vision 14 years after radial keratotomy. Source
Refractive Surgery "Nightmare" Reported to the FDA: RK Followed by PRK
In 1992, i lost my vision after refractive surgery - rk. In early october i had gone to a "free" seminar to gather info before i saw a dr. I had pre-existing scar tissue on my left eye but dr said "no problem", and we proceeded with bilateral refractive surgery. I did not have good vision from the start. I was told that "things have not settled down yet. We can always perform an enhancement. " i struggled with my duties at home and work. In 1993, i went to another city to see another dr -a referral from dr(first)-. He performed a prk on my left eye with later plans to surgically improve the right eye. At that time second dr told me that dr(first) made the cuts in my eyes too deep and too long. My left eye now had vision worse than pre-prk and was covered with scar tissue from the laser. In 1995, i went on medical leave from my surgical nursing position and had a corneal transplant. During that year, i filed for disability retirement. In 1996, i went to jury trial -case, medical malpractice. I was the victim made to look like a perpetrator. We lost the case and threw ourselves into debt. Dr(first) told me i was a good candidate for refractive surgery, that i would have good results and could throw away my glasses. He never told me there was no turning back from this surgery. He never mentioned the star burst, night blindness, double vision or painful dry eye. He never mentioned that i would not be able to care for my three children. I live the nightmare every day and cringe when i see the same advertising today as when i had my disastrous eye surgery. Source
FDA Complaint: Patient Deceived by Surgeon, Misleading Advertising of Refractive Surgery
I was talked into having rk-radial keratotomy- on my eyes by dr. He said, he never had a problem with any of his surgeries and guaranteed me a successful outcome. After the surgery, however, my eyes became very fatigued and sore. He said that i was reading from the twenty-twenty line on the eye chart and that this problem is in my head. He offered no support or guidance in this matter whatsoever, and practically dismissed me. I was shocked. Now i was left with sore, tired, fatigued eyes and no answers, since this was a new procedure in our area. So i began a journey to try and find a solution. This journey has taken me to numerous prominent eye surgeons. The have prescribed soft and hard contact lenses, glasses, performed ck-conductive keratoplasty-, lasik twice, and nothing has really corrected the problem. The pitfalls of corrective eye surgery need to be honestly discussed by these eye doctors, not covered up by misleading advertising and hype. Thank you for your time and concern in this matter. Source
RK Patient Files Report With FDA, Visually Impaired Since 1990
I had the rk surgery done in 1990 and, while the procedure was done years ago, i have decreased vision, halo effect, diminished night vision, and "dehabilitated" daytime vision. Source
Patient Injury Report Filed with FDA: Multiple RK Surgeries, Cataract Surgery, LASIK, and PRK
A surgeon reported concerns with clinical outcomes. A review of patient records provided, indicates one patient exhibited a loss of bcva following lasik surgery in the right eye only. This patient had multiple rk surgeries in the 1980's and 1990's and complained of ghosting, starbursts, halos and difficulty driving at night. He was diagnosed with nuclear sclerotic cataracts and experienced residual hyperoptic astigmatism after the rk surgeries. This patient underwent cataract extraction surgery with an iol implant prior to receiving lasik surgery. The patient's bcva prior to lasik surgery was 20/32. At 5 months post-op, the patient's bcva was 20/30-. A prk enhancement was performed at 13 months post-op lasik. At one month post-op prk enhancement, this patient's bcva was 20/50. Lasik after iol implantation is not an approved indication for this product. Source
"Even in life or death situations, doctors, nurses, and patients all responded to bad incentives. In hospitals in which the reimbursement rates for appendectomies ran higher, for instance, the surgeons removed more appendixes. The evolution of eye surgery was another great example. In the 1990s, the ophthalmologists were building careers on performing cataract procedures. They'd take half an hour or less, and yet Medicare would reimburse them $1,700 a pop. In the late 1990s, Medicare slashed reimbursement levels to around $450 per procedure, and the incomes of the surgically minded ophthalmologists fell. Across America, ophthalmologists rediscovered an obscure and risky procedure called radial keratomy, and there was a boom in surgery to correct small impairments of vision. The inadequately studied procedure was marketed as a cure for the suffering of contact lens wearers. 'In reality,' says Burry, 'the incentive was to maintain their high, often one- to two-million dollar incomes, and the justification followed. The industry rushed to come up with something less dangerous than radial keratomy, and Lasik was eventually born.'"
Michael Lewis. The Big Short: Inside the Doomsday Machine. (2010, WW Norton). pp. 43-44.
Laser in-situ keratomileusis for refractive error following radial keratotomy.
Indian J Ophthalmol. 2011 Jul-Aug;59(4):283-6.
Sinha R, Sharma N, Ahuja R, Kumar C, Vajpayee RB.
Aim: To evaluate the safety and efficacy of laser in-situ keratomileusis (LASIK) in eyes with residual/induced refractive error following radial keratotomy (RK).
Design: Retrospective study.
Materials and Methods: A retrospective analysis of data of 18 eyes of 10 patients, who had undergone LASIK for refractive error following RK, was performed. All the patients had undergone RK in both eyes at least one year before LASIK. Parameters like uncorrected visual acuity (UCVA), best-corrected visual acuity (BCVA), contrast sensitivity, glare acuity and corneal parameters were evaluated both preoperatively and postoperatively. Statistical Software: STATA-9.0.
Results: The mean UCVA before LASIK was 0.16±0.16 which improved to 0.64 ± 0.22 ( P < 0.001) after one year following LASIK. Fourteen eyes (out of 18) had UCVA of ≥ 20/30 on Snellen's acuity chart at one year following LASIK. The mean BCVA before LASIK was 0.75 ± 0.18. This improved to 0.87 ± 0.16 at one year following LASIK. The mean spherical refractive error at the time of LASIK and at one year after the procedure was -5.37 ± 4.83 diopters (D) and -0.22 ± 1.45D, respectively. Only three eyes had a residual spherical refractive error of ≥ 1.0D at one year follow-up. In two eyes, we noted opening up of the RK incisions. No eye developed epithelial in-growth till 1 year after LASIK.
Conclusion: LASIK is effective in treating refractive error following RK. However, it carries the risk of flap-related complications like opening up of the previously placed RK incisions and splitting of the corneal flap.
Complications of small clear-zone radial keratotomy
PURPOSE: To review the postoperative outcome of patients with radial keratotomy who have clear-zone diameters below 2.75 mm.
METHODS: A retrospective review was performed of all patients with radial keratotomy who have clear-zone diameters less than 2.75 mm presenting for consultation from August 1993-September 1995. Preoperative records and surgical reports were reviewed, and a thorough ophthalmic examination was performed.
RESULTS: A total of 37 eyes had a clear-zone size below 2.25 mm. Six eyes were excluded from subsequent analysis due to keratoconus. The remaining 31 eyes had an average clear-zone size of 1.5 mm (standard deviation, 0.4 mm; range, 0.9-2.2 mm). Postoperative morbidity included severe disabling glare in 31 (100%) of 31 eyes, contact lens intolerance in 19 (100%) of the 19 eyes fitted, Snellen visual acuity loss (> 2 lines) in 25 (81%) of 31 eyes, inability to drive at night in 11 (69%) of 16 patients, moderate to severe diurnal visual fluctuation in 21 (68%) of 31 eyes, refractive undercorrection by greater than 1 diopter in 16 (52%) of 31 eyes, loss of employment in 4 (25%) of 16 patients, polyopia in 5 (16%) of 31 eyes, refractive overcorrection by greater than 1 diopter in 3 (10%) of 31 eyes, and a retinal detachment attributable to pilocarpine use in 1 (3%) of 31 eyes.
CONCLUSIONS: Using radial keratotomy clear-zone diameters smaller than 2.25 mm has a high complication rate and is unsafe. Small clear-zone radial keratotomy should be abandoned. Although this study was limited to clear zones less than 2.25 mm, the authors endorse current recommendations that the clear zone should be at least 3.0 mm in diameter.
Source: Grimmett MR, Holland EJ. Complications of small clear-zone radial keratotomy. Ophthalmology. 1996 Sep;103(9):1348-56.
Results of the prospective evaluation of radial keratotomy (PERK) study 10 years after surgery.
OBJECTIVE: To determine the long-term effects and stability of refraction following a standardized technique of radial keratotomy for myopia in the nine-center Prospective Evaluation of Radial Keratotomy (PERK) Study 10 years after surgery.
METHODS: Radial keratotomy using eight centripetal incisions was performed to reduce myopia of -2.00 to -8.75 diopters in 1982 and 1983. A mean of 10 years later, patients underwent a standardized ophthalmic examination similar to previous study examinations.
RESULTS: Of 427 patients (793 eyes that underwent radial keratotomy), 374 patients (88%) (693 eyes) returned for the 10-year examination. Of 675 eyes with refractive data, 38% had a refractive error within 0.50 D and 60% within 1.00 D. For 310 first-operated eyes, the mean refractive error was -0.36 D at 6 months and changed in a hyperopic direction to + 0.51 D at 10 years. The average rate of change was +0.21 D/y between 6 months and 2 years and +0.06 D/y between 2 and 10 years. Between 6 months and 10 years, the refractive error of 43% of eyes changed in the hyperopic direction by 1.00 D or more. The hyperopic shift was statistically associated with the diameter of the clear zone. Uncorrected visual acuity was 20/20 or better in 53% of 681 eyes and 20/40 or better in 85%. Loss of spectacle-corrected visual acuity of 2 lines or more on a Snellen chart occurred in 3% of all 793 eyes that underwent surgery. Among 310 patients with bilateral radial keratotomy, 70% reported not wearing spectacles or contact lenses for distance vision at 10 years.
CONCLUSION: The PERK technique of radial keratotomy eliminated distance optical correction in 70% of patients, with a reasonable level of safety. A shift of the refractive error in the hyperopic direction continued during the entire 10 years after surgery.
Source: Waring GO 3rd, Lynn MJ, McDonnell PJ. Arch Ophthalmol. 1994 Oct;112(10):1298-308.
The Casebeer system for predictable keratorefractive surgery. One-year evaluation of 205 consecutive eyes.
PURPOSE: This study documents the results of current radial keratotomy (RK) surgical technology, using the Casebeer keratorefractive system. These results are contrasted to those of the Prospective Evaluation of Radial Keratotomy (PERK) keratorefractive system, developed approximately 12 years ago.
METHODS: Two hundred five consecutive surgical procedures were examined, which was the first year of experience with RK for one of the authors (TPW). All procedures fit within the Casebeer nomograms. Enhancement procedures were performed following the Casebeer system nomograms.
RESULTS: Follow-up for 100% of patients was achieved. Postoperative cycloplegic refractions yielded an average of +0.27 +/- 0.58 diopters (D) of residual refractive correction (range, -0.88 to +2.50 D). One year postoperatively, 20/25 or better uncorrected visual acuity was achieved in 86% of patients and 20/40 or better uncorrected visual acuity was achieved in 99% of patients. Bothersome but not incapacitating side effects, such as glare, starbursting, and fluctuating vision, have been commonly observed with RK.
CONCLUSION: The Casebeer system for keratorefractive surgery, which is easy to learn, can yield an extremely accurate surgical result. The major reason for increased accuracy compared with the PERK system is the surgeon's ability to titrate the primary surgical procedure with enhancement operations. Although RK is by no means a perfect surgical technique, side effects tend to be relatively minimal, and patient satisfaction tends to be extremely high.
Source: Werblin TP, Stafford GM. Ophthalmology. 1993 Jul;100(7):1095-102.
Corneal ectasia as a complication of repeated keratotomy surgery
BACKGROUND: Staged keratotomy surgery, or "enhancement surgery," may allow a more predictable outcome, but also subjects the patient to additional surgical risks.
METHODS: A 39-year-old man underwent astigmatic keratotomy for myopic astigmatism, followed by 12 enhancement procedures for residual astigmatism.
RESULTS: These procedures effectively resulted in a double hexagonal keratotomy. The patient's best spectacle-corrected acuity deteriorated to counting fingers. Clinically, a conically-shaped protrusion of the central cornea, Munson's sign, diffuse subepithelial scarring, and central corneal thinning were noted. Penetrating keratoplasty was performed. Histopathologic examination showed central thinning, epithelial edema, disruption of Bowman's layer, marked stromal scarring, and focal areas of endothelial attenuation--findings consistent with keratoconus.
CONCLUSION: This case illustrates that multiple keratotomy procedures may result in corneal ectasia in apparently normal eyes and suggests that hexagonal keratotomy may be more likely to cause iatrogenic keratoconus.
Source: Wellish KL, Glasgow BJ, Beltran F, Maloney RK. Refract Corneal Surg. 1994 May-Jun;10(3):360-4.
Iatrogenic keratoconus as a complication of radial keratotomy
A 47-year-old man with a family history of keratoconus had uneventful bilateral radial keratotomy (RK) with astigmatic keratotomy (AK) enhancements 12 years earlier. He noticed a gradual onset of blurry vision with progressively increasing myopic shift. Visual acuity remained poor even with spectacles or soft contact lenses. Slitlamp examination revealed 16 well-healed RK scars and 2 AK scars with marked corneal steepening inferiorly in an area of astigmatic enhancement in the left eye but an otherwise normal fellow eye with 16 well-healed RK scars. He subsequently had penetrating keratoplasty for decreased vision not correctable by rigid gas-permeable contact lenses. Microscopic examination of the corneal button showed findings consistent with keratoconus. This case represents the first documented incidence of corneal ectasia as a complication of primary RK.
Source: Shaikh S, Shaikh NM, Manche E. Iatrogenic keratoconus as a complication of radial keratotomy. J Cataract Refract Surg. 2002 Mar;28(3):553-5.
Complicated flap creation with femtosecond laser after radial keratotomy
PURPOSE: To report a case of laser in situ keratomileusis (LASIK) that used the Intralase femtosecond laser 14 years after radial keratotomy (RK) for residual myopic astigmatism.
METHODS: A 39 year-old male patient had undergone a bilateral RK operation for myopic correction. The manifest refraction was -1.25 -3.00 x 175 D, with uncorrected visual acuity (UCVA) of 20/50 and best-corrected visual acuity (BCVA) of 20/20. The central and thinnest pachymetry measurements were 582 and 576 mum, respectively, by Orbscan II.
RESULTS: Intralase was used for LASIK, and initially, a loss of suction was seen during flap formation. The flap could be created again at the same intracorneal plane. During flap lifting, the RK incisions were separated, and one of the RK incisions progressed to the corneal center with the force applied by the blunt spatula. No piece was separated completely from the flap. Excimer laser treatment and flap repositioning could be done without any problems. At the fifth postoperative month, his UCVA was 20/20. All RK incisions seemed well aligned. There was no haze or epithelial ingrowth.
CONCLUSIONS: This case showed that the Intralase femtosecond laser not only has no unique benefit as opposed to the mechanical keratome for post-RK eyes but also can lead to serious complications. We recommend that femtosecond laser flap formation not be used in post-RK eyes.
Source: Cornea. 2007 Oct;26(9):1138-40. Perente I, Utine CA, Cakir H, Yilmaz OF.
Disclaimer: This information is NOT intended to be used as medical advice. The information contained on this web site is presented for the purpose of warning people about LASIK complications prior to surgery. Persons experiencing vision problems or other eye problems should seek the advice of a physician.
/RK-and-LASIK(320).jpg)
/post-RK_dry_eye(320).jpg)
/post-RK_eye_with_t-cuts(320).jpg)
/2-RK-surgeries_followed_by_LASIK(320).jpg)
/2RK_LASIK_topo_JS_OD(320).jpg)
/2RK_LASIK_topo_JS(320).jpg)
/post-RK_ectasia(320).jpg)
/post-RK_ectasia(320)markedup.jpg)
/post-RK_ectasia_topo(320).jpg)
/corneal-transplant_post-RK_infection(320).jpg)
/RK-incisions(320).jpg)
/post_RK_t-cuts_post_lasik(320).jpg)
/long_RK_incisions(320).jpg)
/postRK_postLASIK_neovascularization(320).jpg)
/postRK_postLASIK_neovascularization_2(320).jpg)
/postRK_postLASIK_neovascularization_3(320).jpg)
.jpg)
.jpg)
.jpg)
.jpg)
.jpg)
/post-RK-ectasia-s.jpg)
/postRK_postlasik(320).jpg)
/2RK_2LASIK.jpg)
/2RK-2LASIK-epi-ingrowth(320).jpg)
.jpg)
/RK_deep_incisions.jpg)
/openRKincisionsOD.jpg)
/postRKectasiaOS.jpg)
/postRKectasia.jpg)
/RK-incision(320).jpg)
.jpg)